Approach Considerations
Treatment of prostatitis should be tailored to symptoms and culture findings and should be supportive. Suprapubic catheterization may be warranted in severe urinary obstruction and should be placed in consultation with a urologist. For further information, the European Association of Urology has treatment guidelines available on chronic pelvic pain and on prostatitis and chronic pelvic pain syndrome. [34, 38]
See the following for more information:
Acute Bacterial Prostatitis
Individuals with acute bacterial prostatitis who are acutely ill, have evidence of sepsis, are unable to voluntarily urinate or tolerate oral intake, or have risk factors for antibiotic resistance require hospital admission for parenteral antibiotics and supportive care. [39] Antibiotic therapy initially should include parental bactericidal agents such as fluoroquinolones, aminoglycosides with or without penicillin derivatives, and third-generation cephalosporins. [40]
Since April 2007, the Centers for Disease Control and Prevention (CDC) has no longer recommended fluoroquinolone antibiotics to treat gonorrhea in the United States. [41, 42] Current CDC treatment guidelines for gonococcal infection recommend single-dose IM ceftriaxone, plus single-dose oral azithromycin or 7 days of oral doxycycline. [42, 18] Co-treatment offers the benefits of hindering the development of antimicrobial resistant gonococci and covering C trachomatis, which often accompanies gonococcal infection.
Patients without a toxic appearance can be treated on an outpatient basis with a 28-day course of oral antibiotics, usually a fluoroquinolone or trimethoprim-sulfamethoxazole. Urologic follow-up is necessary to ensure eradication and to provide continuity of care to prevent relapse.
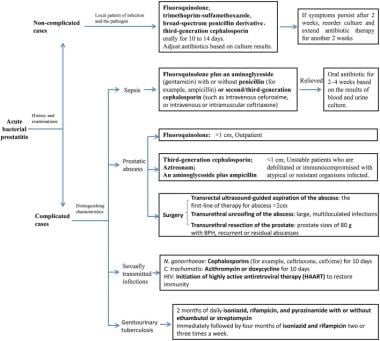 Treatment algorithm for acute bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
Treatment algorithm for acute bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
Urinary retention may complicate acute infection and warrant hospitalization. Suprapubic catheters are considered safer than urethral catheterization in severe obstruction due to prostatic swelling from bacterial infection and may be placed in consultation with a urologist. [43]
Provide supportive measures such as antipyretics, analgesics, hydration, and stool softeners as needed. Urinary analgesics such as phenazopyridine and flavoxate are also commonly used.
Avoid serial examinations of the prostate to avoid seeding of the blood and bacteremia in acute bacterial prostatitis.
In cases of prostatic abscess, the fluctuant site may be drained under local anesthesia either transrectally or transperineally. When performed transperineally, a pigtail catheter can be inserted as a drain. Cystoscopic, transurethral unroofing of an abscess also is possible with the patient under anesthesia.
Chronic Bacterial Prostatitis and Pelvic Pain
A 4- to 6-week trial of antibiotic therapy is indicated in chronic bacterial prostatitis and chronic pelvic pain syndrome with inflammation, but no consensus exists regarding its use in chronic pelvic pain syndrome without inflammation and asymptomatic prostatitis. Recurrences of chronic bacterial prostatitis are common, possibly in part because few antibacterial agents distribute well into the prostatic tissue and achieve sufficient concentrations to eradicate infections. Preferred antimicrobial agents include fluoroquinolones, macrolides, tetracyclines, and trimethoprim. [44] Fluoroquinolones provide relief in about 50% of patients, and treatment is more effective if treatment starts earlier in the course of symptoms. The course of antibiotics can be repeated if the first course provides some relief. [45] A Cochrane review of 18 studies that compared the various fluoroquinolone antibiotics suggested that there were no differences in clinical efficacy or adverse events among them in treating chronic bacterial prostatitis. [44] Fosfomycin has been used to effectively treat multidrug-resistant gram-negative prostatitis. [46]
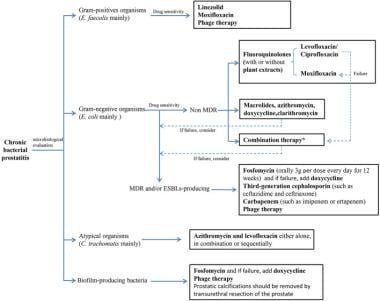 Treatment algorithm for chronic bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
Treatment algorithm for chronic bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
Supportive measures such as analgesics (particularly nonsteroidal anti-inflammatory drugs [NSAIDs]), alpha-blocking agents, hydration, stool softeners, and sitz baths are often used. Alpha-blockers reduce bladder outlet obstruction and thus improve voiding dysfunction that may be associated with prostatic swelling that is common with prostatitis. [47]
Some evidence suggests that pelvic floor training/biofeedback can be effective in controlling the symptoms of chronic prostatitis and chronic pelvic pain syndrome. [21]
In cases where infected prostatic calculi serve as a nidus, transurethral resection or total prostatectomy may result in a cure.
If a patient has received no relief from antibiotics, NSAIDs, and alpha blockade, ensure prompt referral to a urologist.
Carefully treat associated septicemia in acutely ill patients. Carefully monitor for bladder outlet obstruction and renal failure. If urination issues do not resolve and incomplete emptying of bladder urine is suspected, refer the patient to a urologist for an evaluation of urination with flow rate and postvoid assessment of residual urine.
Chronic prostatitis/chronic pelvis pain syndrome (NIH Category III prostatitis) appears to be a collection of clinical phenotypes that may manifest as urinary symptoms, pain, sexual symptoms, and/or psychiatric issues. As a result, it largely has been resistant to monotherapy. Recently, a tailored multimodal approach to this condition has been advocated with success. Based on clinical phenotype, patients are placed into the "UPOINT" system, which classifies symptoms into urinary, psychological, organ-specific, infection, neurologic/systemic, and tenderness domains. [48] Based on the patient-specific symptom domains, multimodality therapy that is tailored to each patient is prescribed.
Prevention of Prostatitis
Protection against sexually transmitted diseases (STDs) also provides protection against many organisms associated with acute bacterial prostatitis, development of chronic prostatitis, and suspected causes of nonbacterial prostatitis.
Psychological stress has been associated with men who report symptoms of chronic prostatitis. [15, 4] Recognition of underlying psychosomatic disease in chronic cases and appropriate psychiatric referral and treatment lessen the recurrence rate.
Consultations
After primary management and stabilization of the patient with acute prostatitis, care is appropriately transferred to a urologist.
Aggressive treatment can lessen the chance of developing chronic prostatitis. Chronic bacterial prostatitis, chronic pelvic pain syndrome, and asymptomatic inflammatory prostatitis also are probably best treated by or in consultation with a urologist.
Notify the health department if a reportable STD is documented. Consult a psychiatrist if psychosomatic disorder is suspected.
Long-Term Monitoring
After initial improvement with parental antibiotics, acute bacterial prostatitis may be managed with outpatient care with a 2- to 4-week course of oral antibiotics and urologic follow-up. Management strategies for category II prostatitis, chronic bacterial prostatitis, include intraprostatic antibiotic injection, alpha-blocker therapy, transurethral resection of the prostate (TURP), and long-term antimicrobial suppression.
Additional therapeutic modalities studied for category III prostatitis include anti-inflammatories, phytotherapy, biofeedback, thermal therapy, and pelvic floor exercises.
Prostate-specific antigen (PSA) levels may be elevated with both prostatitis and prostate cancer. However, PSA levels typically fall after resolution of prostatitis but do not fall with prostate cancer. Patients found to have elevated PSA levels should have follow-up by their primary care physician, urologist, or both.
PSA levels may increase with acute prostatitis; with appropriate antibiotic treatment, levels usually return to normal within 1-3 months. [49] In some studies, a longer course of antibiotics has been shown to result in a decrease in PSA values in patients with category IV prostatitis.
-
Bacterial prostatitis. Expressed prostatic fluid contains more than 10 white blood cells per high-power field, indicating prostatitis.
-
A nonspecific mixed inflammatory infiltrate that consists of lymphocytes, plasma cells, and histiocytes is typical in chronic bacterial prostatitis.
-
Urine culture with greater than 100,000 colony-forming units (CFU) of Escherichia coli, the most common pathogen in acute and chronic prostatitis. Chronic bacterial prostatitis must be confirmed and diagnosed using a urine culture.
-
Treatment algorithm for chronic bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
-
Treatment algorithm for acute bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].








